Mpox outbreak: Aceng rebukes misinformers
Aceng reassured Ugandans that the outbreak is under control. “We continue to monitor and contain the disease.
Minister of Health Dr. Jane Ruth Aceng provided the latest update on Mpox during the discharge ceremony for all Ebola patients on Wednesday, February 18th. (Credit: John Musenze)
By NewVision Reporter
Journalists @NewVision
By John Musenze
KAMPALA - Uganda’s health ministry says 2,126 mpox patients have recovered from mpox after receiving supportive treatment at Entebbe Isolation Facility and other public health centres.
Health minister Dr Jane Ruth Aceng while providing an update, has also addressed misinformation circulating about the outbreak, particularly from social media and video bloggers.
“There is no ministry that can declare an outbreak when there is none. Controlling outbreaks is not a matter of seeking funds; it is about saving lives. We condemn such reckless statements and urge the public to rely on official Ministry of Health sources for accurate information,” she says.
She was giving the health ministry's latest update on Mpox during the discharge ceremony for all Ebola patients on February 18, 2025. Aceng said 87 districts have reported at least one confirmed Mpox case, with a total of 2,896 confirmed cases.
Unfortunately, 19 individuals succumbed to the disease, with the majority of deaths occurring among patients with underlying conditions such as HIV, tuberculosis, and sickle cell disease.
“All public health facilities across the country act as sample collection points for patients who present with signs and symptoms consistent with mpox disease,” Aceng stated.
Since the outbreak was declared, the National Isolation Facility in Entebbe has served as the primary treatment centre. As of January 31, 2025, a total of 1,589 patients had received supportive treatment, recovered, and been discharged.
“We have implemented active case searches, contact tracing, public awareness campaigns, and training for health workers. Our National Isolation Facility in Entebbe remains the primary treatment centre, where 1,589 patients have been treated and discharged,” she said.
Aceng reassured Ugandans that the outbreak is under control. “We continue to monitor and contain the disease. There are no restrictions on gatherings, trade, or travel. Uganda remains safe, and we have the capacity to manage any outbreak.”
Vaccine rollout and future plan
To ease the burden on the Entebbe facility, the health ministry has introduced home-based care for mild cases.
Additionally, Uganda received 10,000 doses of the Mpox vaccine, with 9,980 doses already administered to high-risk groups, primarily commercial sex workers in Kampala.
Dr. Henry Sendikaddiwa, the Mpox response lead at Nakasongola Health Centre IV, recalled the initial struggles. (Credit: John Musenze)
Aceng announced that the African Centres for Disease Control (CDC) has pledged an additional 100,000 vaccine doses to further support Uganda’s response.
“It is important to note that the category of commercial sex workers receiving the vaccines includes both males and females. We strongly believe that vaccination will play a crucial role in interrupting transmission, preventing severe illness, and reducing mortality due to Mpox,” she stated.
A frontliner’s perspective
Dr Henry Sendikaddiwa, the Mpox response lead at Nakasongola Health Centre IV, recalled the initial struggles.
“At the beginning, there was no money, no guidelines, and no extra staff. We had to fund the first few cases from our own pockets, providing food and medicine. I had to reassign existing staff to handle mpox cases permanently because we couldn’t risk cross-contamination,” he explained.
Sendikaddiwa described the severity of early cases: “You would open up a wound, and everything was eaten away by pus. We stood firm as a team, provided what little we could, and called on organisations like WHO and the health ministry to step in.”
The lack of isolation units posed another challenge: “Mothers with young children were particularly difficult cases. We had to improvise, creating separate sections within tents to accommodate families. Miraculously, none of the children got infected”.
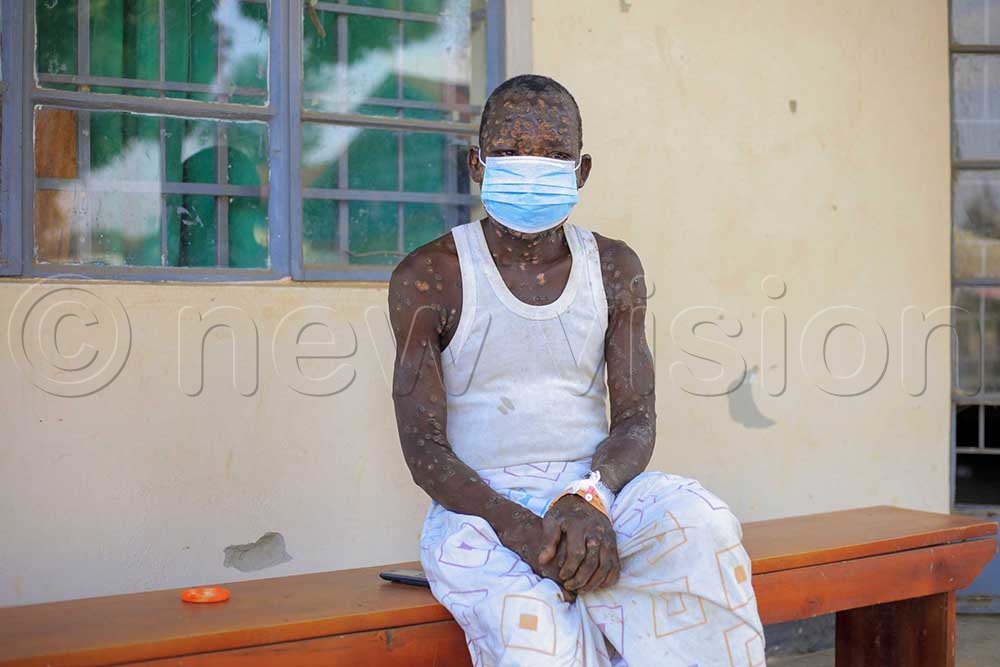
Mpox patient at Nakasongola district Isolation center. (Credit: John Musenze)
Despite these struggles, the team remained resilient. “At first, we had no standard treatment protocol, but over time, we gained experience. We saw everything—from mild cases to the most severe. Some patients had no skin left on their bodies”.
With time, support from WHO and the health ministry improved conditions. “Now, WHO provides fuel for patient transportation, and the Ministry supplies meals. The situation has stabilized, but the lessons remain.”
The need for long-term preparedness
Sendikaddiwa emphasized the need for long-term preparedness. “We need permanent isolation units and continuous training for health workers. Outbreaks like Mpox and COVID-19 have shown that we must always be ready.”
Uganda’s mpox fight: a six-month battle
On July 24, 2024, Uganda declared Mpox outbreak following confirmation of two cases from Mpondwe. Since then, the country has fought a six-month battle against the disease, with 87 districts reporting confirmed cases.
As of January 31, 2025, the health ministry has recorded 2,896 confirmed cases, with 19 fatalities. The majority of those who died had pre-existing health conditions. However, due to rigorous containment efforts and supportive treatment, 2,126 patients have successfully recovered.
With the upcoming arrival of 100,000 additional vaccine doses from the African CDC and strengthened healthcare measures, Uganda remains committed to controlling the outbreak and ensuring long-term readiness against future public health threats according to Aceng.
